Iron deficiency anemia
IRON DEFICIENCY ANEMIA
Iron deficiency is a common nutritional deficiency in the world. Iron is important for hemoglobin synthesis. Not only that, Iron is required for many other important cellular functions.
So, what is Iron deficiency Anemia? Before discussing the iron deficiency anemia, we must first understand that how Hb is synthesized inside the RBCs and how RBCs are synthesized. And what is the role of iron in this process.
All the blood cells are born from a single type of cells in bone marrow of an adult. The cells are called Pluripotent hematopoietic stem cells. These cells replicate. Some of these replicated cells remain there to keep a supply of these stem cells. While other differentiate into cells that are committed towards formation of a specific blood cell progeny. For example, some will synthesize WBC, some will synthesize megakaryocytes and so on. But we are concerned with RBC here. Those committed stem cells that form RBCs are called Colony Forming Unit-Erythroblast (CFU-E) because they rapidly divide form colonies of RBC Forming Cells.

Before moving forward, let's discuss briefly the structure of Hb
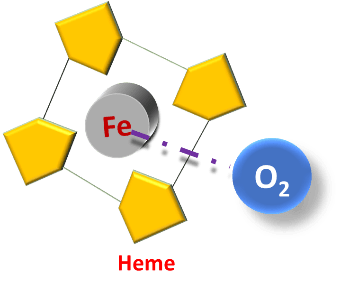
Heme consists of a protoporphyrin ring. This Protoporphyrin ring surrounds a Ferrous (Fe2+) ion. This Protoporphyrin ring along with the Iron is called heme.
This Fe2+ can then reversibly bind oxygen thus performing its function of transport of oxygen.
The other component is globin which is a protein synthesized like another protein by transcription followed by translation of globin gene.

Hemoglobin is a tetramer of four such subunits
(Heme + Globin)
From CFU-E under appropriate stimulation large nucleated erythroblasts are formed.
In the Mitochondria through multistep process Protoporphyrin ring is formed, it now needs a supply of Iron, which it will incorporate into the Protoporphyrin ring, thus forming heme.
60700eb17e917_lg.png)
This heme will then combine with globin chains to form hemoglobin. If Iron isn’t supplied adequately, Iron won’t be incorporated into Protoporphyrin rings and heme (and thus hemoglobin will not be formed. This Free Protoporphyrin will start accumulating in the RBC.
Protoporphyrin act as an oxidant and can generate Reactive oxygen species (ROS). ROS are generally detoxified by iron-requiring enzymes (Glutathione peroxidase and catalase). In Iron deficiency, such enzymes are deficient. So, there will be ROS mediated lipid peroxidation of the RBC’s plasma Membrane. [1] This leads to mis-shaped RBCs (elliptical cells, target cells etc.) with decreased flexibility.[2] Furthermore, the life span of RBC in Iron deficiency is reduced[3]
Now where this supply of iron comes from? Well there are some special trucks that transport these ferrous ions from the source of iron to the site where it is to be utilized (erythroblasts of the bone marrow, for example). And these ferrous transporting proteins (trucks) are called Transferrins. They are loaded with ferrous ions. How they are loaded with iron we will discuss that latter.
60700f3e02c40_lg.png)
The early erythrocyte progenitor cells have very little hemoglobin and as they divide and become more specialized, more and more hemoglobin start accumulating in them and with each division of erythroblast progeny they become smaller and smaller in size and continue to accumulate hemoglobin and that will impart red color to it.
But Erythrocytes are selfish cells like some thankless people in our society. As they continue to mature they start throwing out the people who have created hemoglobin for them. i.e. They start throwing out nucleus and most of the organelles, including ribosomes and mitochondria. But probably it’s a necessary evil. They do so in order to keep their size smaller so as to easily pass through the narrow passageways of capillaries and lest they should get stuck in the capillaries and will be engulfed by hostile monsters i.e. Macrophages.
606dc9ef87feb_lg.png)
If due to any reason iron supply is compromised, the heme and thus hemoglobin won’t form adequately so erythroblasts progeny will continue to divide and sub-divide in the hopes that more Hb will be accumulated into it. But because Iron supply is less, Hb will remain low, nonetheless as the cells continue to divide they become smaller in size. The RBCs thus formed are less red in color (hypochromic) and smaller in size (Microcytic) then the normal RBCs.
Now let’s come to discussion of where this Iron for heme synthesis comes from?
Iron comes from two sources
1. Dietary iron from intestinal epithelial cells
2. From a graveyard – A graveyard, you may wonder.
606dcf23257f4_lg.png)
Dietary Iron from plant sources is in the ionic form. Phytic acid and other components of vegetarian diet including oxalates and phosphates form insoluble complexes with Iron and other minerals and impairs their absorption. Animal based diet has iron in the form of heme. Heme iron has better absorption. Thus, vegetarians are more prone to develop iron deficiency in long run.
Most of the non-heme iron is in ferric form (Fe3+). On the apical side (luminal side) of duodenal enterocytes there is a special enzyme which reduces ferric iron to ferrous iron called ferric reductase as Iron is absorbed in the ferrous form. Vitamin C and stomach acid also helps to keep iron in reduced form. This ferrous Fe2+ is then transported inside the enterocyte by Divalent Metal Transporter 1 (DMT1) transporter protein. Which is not loyal to iron, it is also involved in absorption of other divalent ions e.g. Cu2+
606dd0ca194a5_lg.png)
Hey, By the way how can you remember ferrous and ferric ion. Ferric ion is Fe3+. Ferric rhymes with hat-trick. While ferrous is Fe2+ and ferrous has ‘O’ in it as twO has O in it.
Heme, on the other hand is transported into the cell as such by Heme Carrier protein 1 (HCP1). Inside the cell Fe2+ is released from the heme by Hemeoxygenese 2 enzyme. [4]
This ionic iron (Fe2+), that is obtained from heme as well as non-heme dietary source is toxic to cell. It may form oxide radicals. Thus, it is immediately thrown into tin packs specialized to store the ferrous. These proteins are called Ferritin.
It consists of a spherical shell of protein called ApoFerritin, the center core of this ApoFerritin is filled with iron and this structure as a whole (Apoferritin + Iron) is called Ferritin.
606ec1c2c6376_lg.png)
Ferritin is the storage form of iron. Almost 25-30% of iron in our body is in the form of ferritin. Ferritin is intra-
606edfa9136db_lg.png)
cellular cytosolic protein present in small amount in all cells but mainly found in macrophages of bone marrow and spleen, Hepatocytes and enterocytes.
Despite of being intracellular protein, small amounts of ferritin is secreted by bone marrow macrophages into the plasma.
606ee132d4d43_lg.png)
And this plasma (serum) ferritin level directly correlates quantitively with the bone marrow macrophages’ ferritin. This serum ferritin levels are routinely measured in laboratory as a part of serum iron studies to estimate the iron stores. Though exact role of the serum ferritin remains poorly understood.
As per requirement ferrous is removed from the ferritin and ported out of the cell at the basal side of enterocyte
606ee2c95d2e4_lg.png)
with the help of a carrier protein called ferroportin. Here there are some empty trucks which are sent by Liver to pick up this iron and transfer it to wherever it is required. These empty trucks specialized in transporting the ferrous are called ApoTransferrin. And when they are loaded with iron they are called transferrin.
Transferrin carry the iron mainly to bone marrow erythroblasts for hemoglobin synthesis and to the liver for synthesis of some other components for example Cytochromes, Peroxidase and catalases.
When excess of Iron is present in the body, Liver will synthesize hepcidin protein which will internalize the ferroportin protein thus preventing excessive iron absorption.
606ee4fa71e96_lg.png)
It’s noteworthy that there is no precise and well-coordinated mechanism to excrete extra iron that has once been absorbed into the body. The only way body gets rid of iron under physiological conditions is through shedding of enterocytes filled with iron during normal cellular turnover and in females during menstruation. Small amount of iron is also lost during normal turnover of skin cells as well as during sweating.
Under pathological conditions iron is only lost when blood is lost from the body. i.e. external hemorrhage.
So, in a nutshell, Iron is imported into our body from the deep seas of intestinal lumen via the ships of enterocyte and ported into the blood via the seaport of ferroportin and transported onto the roads of blood vessels via the transferrin trucks.
606ee69f54dc4_lg.png)
The other source of iron is graveyard… Ohhh.. Not the ordinary graveyard.. It’s the graveyard of RBCs. Spleen, my friends.
In the red pulp of Spleen there are specialized blood capillaries with gaps in the them. These specialized capillaries are called sinusoids. Young and healthy RBC can come out from these sinusoids and can go back into them by squeezing themselves through these gaps. They are flexible enough due to some special membrane proteins which maintain their flexibility. The old, fragile RBC that cannot squeeze through these sinusoids and gets stuck there because they are not flexible enough. The proteins responsible for maintaining the flexibility becomes dysfunctional with time. Now karma has caught them, they had thrown out their protein synthesizing machinery i.e. Nucleus, ribosomes and other organelles and now they are stuck in the Death Valley of spleen as they can no more synthesize their flexibility maintaining proteins. They are eaten up by the horrific monsters, I mean, macrophages in the spleen.
606ee90d18c12_lg.png)
These macrophages will release the iron from heme of these RBC. This Iron is stored in soluble ferritin. Sometimes excess of iron overwhelms the storage capacity of the ferritin so iron is stored in the form of insoluble ferritin aggregates called hemosiderin. From Macrophages the iron can be mobilized to wherever required, by utilizing its very own truck à Transferrin.
This source of iron from spleen is recycled iron. It’s that iron which is obtained from recycling of iron from dead RBC’s hemoglobin.
Etiology of Iron Deficiency:
Iron deficiency occurs when there is:
1. Increased requirement
a. Toddlers and infants -Increase iron requirement + Breast milk is deficient in iron
b. Children and adolescents- Increase requirement due to growth
c. Pregnancy
2. Decreased supply
a. Vegetarian diet, as it contains some compounds like phytates that impede iron absorption.
b. Malnutrition
3. Increase losses
a. Chronic blood loss (e.g. APD, hookworm infestation) b. Menorrhagia
606ee9f7407db_lg.png)
Clinical features:
Now that we have understood that how Iron deficiency occurs and how it can lead to anemia. Now we will look into what problems it can lead to:
In Iron deficiency anemia, RBC are Hemoglobin deficient, so they are bringing less then normal Oxygen to the peripheral tissues. Myoglobin is the heme containing pigment in muscle that acts as reservoir of oxygen and can release its own oxygen for muscle to use when supply of oxygen externally from blood is impeded so that muscle would sustain oxygen deficient circumstances for longer.
Myoglobin would be deficient in Iron deficiency. Energy is obtained in the form of ATP; the energy currency, from Glucose by the process of Glycolysis and pyruvate is formed. Furthermore, Bank cheques are obtained in the form of NADH and FADH2. These cheques are withdrawn from the
bank of Respiratory chain by oxidative phosphorylation (an oxygen dependent process). Here again some more ATP molecules are obtained. Components of respiratory chain (cytochromes) require oxygen. Our body loves to suck out every penny possible from the nutrients, so Pyruvate is
then funneled through the TCA cycle to obtain some more ATPs are obtained (again, it’ O2 dependent pathway).
6070244ca112f_lg.png)
Hemoglobin is required for Oxygen transport so in any anemia (including Iron deficiency) oxygen demand of the tissue won’t be met adequately and there will be inadequate tissue oxygenation so patient will complain of:
- Tiredness and lethargy
- Dyspnea (breathlessness) on exertion
- Headache;
Sympathetic system will try to compensate by increasing the heart rate thus leading to tachycardia and palpitation. Anemia can exacerbate pre-existing cardiopulmonary problems e.g. Angina and Intermittent claudication especially in elderly.[5]
The red color of blood is due to presence of hemoglobin. Since Hb decreases in anemia there will be generalized pallor especially evident from mucus membrane and conjunctiva of the eye.
606ffcebe930d_lg.png)
6070250ccee1b_lg.png)
Remember, Iron is not only required for synthesis of Hemoglobin, but it has many other roles. Iron also act as co-factor for many enzymes, Ribonucleotide reductase is one of them. This is enzyme is required to form Deoxyribonucleotides which are essential for DNA synthesis. It means when iron is deficient mitotic activity of cells will decrease due to depletion of Ribonucleotide reductase[6] [7]. Rapidly proliferating cells suffer the most. GIT epithelium is a classical example. GIT epithelium is routinely shed into the lumen and new epithelium is continuously being formed.
In Iron deficiency anemia, GIT epithelium isn’t efficiently replaced so there are manifestations like atrophy of papillae of tongue (flattening/smoothening of tongue) as well atrophic gastritis. Angular stomatitis (inflammation of corners of mouth) is also seen in some patients of iron deficiency anemia.
60702611b986c_lg.png)
Furthermore, depletion of iron-containing enzymes in the cells might also be the cause of such manifestations in iron deficiency.
How koilonychia develops in Iron deficiency anemia:
Nail plate consists of fibrous keratin proteins arranged parallel to its transverse axis.[8] [9] These keratin fibers are held together by non-fibrous globular proteins. These globular proteins are rich in cystine which forms the disulfide bond with keratin thus acting as a glue. These disulfide bonds impart strength and integrity to nail plate[10]
606ffe283c451_lg.png)
Cysteine is semi-essential amino acid that can be synthesized in body from methionine through a multi-step process involving many enzymes.[11] One of these enzymes is heme-containing[12] [13] cystathionine beta-synthase[14], that might be deficient in iron deficiency anemia. This might be the reason for decrease is cystine content of nail in iron deficiency.[15] [16] When cystine is deficient the strength and integrity of nail plate is not maintained, and this leads to thin and brittle nail in iron deficiency anemia.
606fff1111ee4_lg.png)
Furthermore, it is believed that iron deficiency anemia leads to decreased oxygenation of distal part of the subungual connective tissue (connective tissue below the nail bed).[17] [18]
606fffcd6e5f3_lg.png)
Due to which the thin brittle nail plate is everted from the margins with a central depression or concavity thus adopting a spoon like shape.[19] This condition of nail is called Koilonychia and is characteristic of iron deficiency anemia. Perhaps the pathogenesis of this condition is not that simple. Most of the aspects of it aren’t completely understood yet.
Iron is part of enzymes required for synthesis of certain neurotransmitter in the brain including serotonin and dopamine.[20] Thismight be the reason for development of PICA and restless leg syndrome in some patients with iron deficiency [21]
Pica is an eating disorder that involves eating non-food
607002b3e5b4e_lg.png)
items, such as hair, dirt, ice and paint chips. Pica is derived from the Latin word for the magpie (pica pica), a bird that gathers variety of non-food items[22]
Restless leg syndrome is a disorder characterized by an often unpleasant or uncomfortable urge to move the legs that occurs during periods of inactivity, particularly in the evenings, and is transiently relieved by movement.
In a nutshell, Clinical features Iron deficiency anemia consists of:
Erythroid clinical features (due to decrease Hb):
- Lethargy
- Dyspnea on exertion
- Tachycardia
- Palpitation
- Pallor
Non-Erythroid clinical features:
- Brittle nails
- Koilonychia
- Angular stomatitis
- Atrophic Glossitis
- Atrophic gastritis
- PICA
- Restless leg syndrome
Investigations:
- Complete Blood Count:
a. Since Iron is required for Hb synthesis there will be:
i. Low Hb
ii. An average Red Blood cell will have less than normal hemoglobin concentration. Normally, An RBC is 1/3rd full of Hemoglobin. In order words, Mean Corpuscular Hemoglobin concentration is about 33% (100%/3). But in Iron deficiency anemia there will be low MCHC (Mean Corpuscular Hemoglobin concentration) and Mean Corpuscular Hemoglobin (MCH)
- 1. Raised Free Protoporphyrin Levels:
- a. The incorporation of iron into protoporphyrin represents the ultimate stage in the biosynthetic pathway of heme. Failure of iron supply will result in an accumulation of free protoporphyrin not incorporated into heme synthesis in the normoblast and the release of erythrocytes into the circulation with high FEP levels.[i]
- 1. Peripheral Smear:
6070054fad2e9_lg.png)
- a. Microcytic Hypochromic Erythrocytes:
- i. Normally an RBC is 1/3rd full of Hemoglobin and there is central 1/3rd area of pallor and rest of the RBC is red due to presence of Hb but in Iron deficiency the area of pallor is increased and Hb is confined merely to a peripheral rim.
- a. Pencil cell/Cigar cells/Elliptocytes
- i. ROS mediated membrane damage leads to abnormally shaped Elliptical cells characteristically seen in Iron deficiency anemia. They are sometimes called Pencil cells or cigar cells due to such resemblance.
- 1. Bone Marrow Biopsy:
- a. Bone marrow biopsy is gold standard but is rarely required for diagnosis[i]
2. Iron Studies
a. Serum Ferritin
i. Serum Ferritin is the storage form of Iron. Although it is present all cells but mainly found in Bone marrow macrophages, Intestinal epithelial cells and Hepatocytes. Macrophages are the primary site for storage of Iron in the form of ferritin in bone marrow. But measurement of bone marrow’s ferritin level isn’t feasible. Small amounts of ferritin are secreted by macrophages into the plasma[ii]. This serum level directly corelates with the ferritin stores in the macrophages[iii]. In Iron deficiency states, cells require Iron which is already deficient in plasma so body will try to empty the iron stores. So, Macrophages Ferritin level will be decreased which will also be manifested as decrease in Serum ferritin level
- a. Serum Iron:
i. In serum, Iron is bound to the Transferrin (remember the trucks used to transport iron). This Transferrin-bound Iron is depicted as Serum Iron in Iron studies. In Iron deficiency anemia Serum Iron level will be obviously low
As Iron is low in the body and Iron demand of cells is not being met, Our Master chemist, the worthy liver, will send a lot of empty trucks (ApoTransferrin) to the intestine and RBC Graveyard (Spleen) to fetch every possible Iron
b. Serum Transferrin & TIBC: Increased
i. As Iron is low in the body and Iron demand of cells is not being met, Our Master chemist, the worthy liver, will send a lot of empty trucks (ApoTransferrin) to the intestine and RBC Graveyard (Spleen) to fetch every possible Iron
- atom but these trucks will mostly return empty because Iron is low.
- ii. This is indicated by increase in number of seats on which Iron can sit. And this is called Total Iron Binding capacity. The TIBC of blood is the amount of iron held by the serum when the iron transport proteins are completely saturated. It indirectly reflects the quantity of serum transferrin[i] [ii]
607006e5c3406_lg.png)
a. Iron Saturation:
1. Percentage of iron bound to transferrin
2. In Iron deficiency anemia Transferrin saturation will be low
References
[1] S K Jain, R Yip, R M Hoesch, A K Pramanik, P R Dallman, S B Shohet, Evidence of peroxidative damage to the erythrocyte membrane in iron deficiency, The American Journal of Clinical Nutrition, Volume 37, Issue 1, January 1983, Pages 26–30, https://doi.org/10.1093/ajcn/37.1.26
[2] Yip, R., Mohandas, N., Clark, M., Jain, S., Shohet, S., & Dallman, P. (1983). Red cell membrane stiffness in iron deficiency. Blood, 62(1),
[3] Enika Nagababu, Seema Gulyani, Christopher J. Earley, Roy G. Cutler, Mark P. Mattson & Dr Joseph M. Rifkind (2008) Iron-deficiency anaemia enhances red blood cell oxidative stress, Free Radical Research, 42:9, 824-829, DOI: 10.1080/10715760802459879
[4] “Gastrointestinal Physiology.” Ganong's Review of Medical Physiology, by William F. Ganong and Kim E. Barrett, McGraw Hill Education, 2016, pp. 484–485.
[5] “Anemia: An Introduction.” Kumar & Clark's Clinical Medicine, by Parveen Kumar et al., Elsevier, 2017, p. 521.
[6] Hoffbrand, A. V., Ganeshaguru, K. , Hooton, J. W. and Tattersall, M. H. (1976), Effect of Iron Deficiency and Desferrioxamine on DNA Synthesis in Human Cells. British Journal of Haematology, 33: 517-526.
[7] Heath, J.L.; Weiss, J.M.; Lavau, C.P.; Wechsler, D.S. Iron Deprivation in Cancer––Potential Therapeutic Implications. Nutrients 2013, 5, 2836-2859.
[8] De Berker, D. A. R., André, J., & Baran, R. (2007). Nail biology and nail science. International journal of cosmetic science, 29(4), 241-275.
[9] Forslind, B. (1970). Biophysical studies of the normal nail. Acta dermato-venereologica, 50(3), 161.
[10] “Chapter 22: Tissue Proteins and Body Fluids.” BIOCHEMISTRY, by DR U. CHAKRAPANI U. SATYANARAYANA, third ed., ELSEVIER INDIA, 2013, p. 490.
[11] “Metabolism of Proteins and Amino Acids.” Harper's Illustrated Biochemistry, by Robert K Murray, 29th ed., Appleton & Lange, 2012, pp. 292–293.
[12] Kery, V., Bukovska, G., & Kraus, J. P. (1994). Transsulfuration depends on heme in addition to pyridoxal 5'-phosphate. Cystathionine beta-synthase is a heme protein. Journal of Biological Chemistry, 269(41), 25283-25288.
[13] Meier, M., Janosik, M., Kery, V., Kraus, J. P., & Burkhard, P. (2001). Structure of human cystathionine β‐synthase: a unique pyridoxal 5′‐phosphate‐dependent heme protein. The EMBO Journal, 20(15), 3910-3916.
[14] McBean, G. J. (2012). The transsulfuration pathway: a source of cysteine for glutathione in astrocytes. Amino acids, 42(1), 199-205.
[15] Jalili, M.A. and Al-Kassab, S. Koilonychia and cystine
content of nails. Lancet1,108 (1959)
[16] Lansdown, A. B. G. (2001). Iron: a cosmetic constituent but an essential nutrient for healthy skin. International journal of cosmetic science, 23(3), 129-137.
[17]Stone OJ. Clubbing and koilonychia. Dermatol Clin 1985; 3: 485–490.
[18] Walker, J., Baran, R., Velez, N., & Jellinek, N. (2016). Koilonychia: an update on pathophysiology, differential diagnosis and clinical relevance. Journal of the European Academy of Dermatology and Venereology, 30(11), 1985-1991.
[19] Takahashi, T., Yamashita, K., & Hatao, K. (2010). Incidence of koilonychia and atrophy of the lingual papillae in a patient with iron-deficiency anemia. International journal of hematology, 91(2), 161-162.–
[20] Youdim, Moussa & Yehuda, Shlomo & Ben-Shachar, Dorit & Ashkenazi, R. (1982). Behavioral and brain biochemical changes in iron-deficient rats: the involvement of iron in dopamine receptor function. Iron Deficiency: Brain Biochemistry and Behavior. 39-56.
[21] Brigo, F., Vogrig, A., Bratti, A., Tavernelli, V., Nardone, R., & Trinka, E. (2018). Probable dysimmune epilepsia partialis continua manifesting as epileptic moving toes syndrome: electroclinical features of a challenging case. Epileptic Disorders, 20(4), 301-312.
[22] Johnson BE. Pica. In: Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd edition, Walker HK, Hall WD, Hurst JW (Eds), Butterworths, Boston 1990.
[23] Goljan, E. F. (2014). Rapid review pathology (Fourth edition.). Philadelphia, PA: Elsevier/Saunders. P. 290.
[24] Ho CH. White blood cell and platelet counts could affect whole blood viscosity. J Chin Med Assoc. 2004 Aug;67(8):394-7. PubMed PMID: 15553798
[25] Lanzkowsky, Philip. Manual of Pediatric Hematology and Oncology. London: Academic Press; 2005. p. 74.
[26] “Hematologic Diseases and Neoplasms.” Step-up to Medicine, by Steven S. Agabegi et al., 4th ed., Wolters Kluwer, 2016, p. 329.
[27] Cohen, L. A., Gutierrez, L., Weiss, A., Leichtmann-Bardoogo, Y., Zhang, D., Crooks, D. R., Sougrat, R., Morgenstern, A., Galy, B., Hentze, M. W., Lazaro, F. J., Rouault, T. A., & Meyron-Holtz, E. G. (2010). Serum ferritin is derived primarily from macrophages through a nonclassical secretory pathway. Blood, 116(9), 1574-1584.
[28] James D. Cook, David A. Lipschitz, Laughton E. M. Miles, Clement A. Finch, Serum ferritin as a measure of iron stores in normal subjects, The American Journal of Clinical Nutrition, Volume 27, Issue 7, July 1974, Pages 681–687
[29] Morgan EH: Transferrin and transferrin iron. IN Iron Biochemistry and Medicine, Jacobs A, Worwood M (eds). London, Academic Press, 1974, pp 29-71
[30]
Brown EB: Transferrin: physiology and function in iron transport.
 Dr. Aizaz
Dr. Aizaz